DictionaryMelanomaMelanomaFemale, 46 years, Nodular malignant melanoma, tumor thickness 3,7 mm 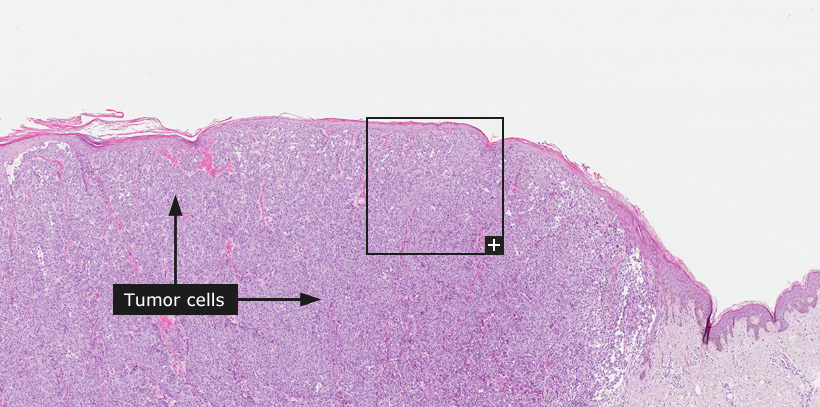
MelanomaMalignant melanoma is the leading cause of skin-related death in Caucasians, but rare in populations with darker pigmented skin color. The incidence has increased dramatically during the last decades, with an almost four-fold increase in the Nordic countries during the time period 1964-2003. The increased incidence reflects in part different sun exposure habits in the population, but hereditary risk factors including skin type are also important. Short intermittent exposure with sunburns appears to be the main risk factor. Other important risk factors include the number of melanocytic nevi and the number of dysplastic melanocytic nevi. Patients that present with an advanced tumor stage at time for diagnosis and patients with relapse of melanoma after surgical removal generally have a poor prognosis. In patients diagnosed with localized disease, the most important prognostic indicator is the thickness of the tumor at the time of diagnosis. The tumor thickness is measured in mm (according to a system initially described by Breslow) and is the dominating parameter for determining the tumor stage (T-stage) of melanoma. Other prognostic factors include mitotic rate and ulceration as well as clinical factors such as patient age, gender and the anatomic site of the primary tumor. In Sweden, the 5-year melanoma specific survival rate is 98% for patients in stage IA (tumor thickness <1 mm and without ulceration and 49% for patients in stage IVB (tumor thickness >4 mm and with ulceration). Primary cutaneous malignant melanoma is thought to develop in a multi-step process. Precursor lesions, such as dysplastic melanocytic nevi develop into a melanoma in situ stage and further into invasive melanoma and eventually metastatic melanoma. Invasive malignant melanoma is traditionally divided into four principal histopathological subgroups based on the microscopical appearance: superficial spreading melanoma (SSM), nodular malignant melanoma (NMM), lentigo maligna melanoma (LMM) and acral lentiginous melanoma (ALM). The histopathological features of malignant melanomas vary widely. A typical feature, often facilitating the diagnosis of melanoma, is the presence of a pagetoid growth pattern. Pagetoid growth pattern is characterized by growth of melanoma cells in the upper layers of the epidermis (as opposed to the localization of normal melanocytes in basal layers of the epidermis). The melanoma cells can be large and rich in cytoplasm, small or even spindly. In a subset of melanomas there are areas with abundant melanin and in other melanomas melanin pigment is scarce or absent. Tumor cell nuclei are enlarged, often with a prominent nucleolus and mitoses are present at a variable degree. Immunohistochemistry is often used to distinguish malignant melanoma from other tumor types. Traditionally, antibodies towards different S100 proteins have been used as immunohistochemical markers of melanocytes, however, antibodies also stain positive in e.g. Langerhans cells and nerve fibers. Other markers such as Melan-A (MART1,MLANA) and tyrosinase (TYR), stain melanocytes more specifically and are useful to determine if a tumor is of melanocytic origin. Proliferation markers are also widely used in the differential diagnostics of melanocytic lesions with uncertain malignant potential. The most accepted markers for cells active in the cell cycle are antibodies binding to Ki-67 (a href='/ENSG00000148773-MKI67/tissue'>MKI67) and the presence of Ki-67 positive melanocytic cells is often used in routine pathology to distinguish malignant melanoma from benign melanocytic tumors.
Normal tissue: Skin |